Lower-extremity muscle atrophy and fat infiltration after chronic spinal cord injury.
J Musculoskelet Neuronal Interact, 2015; 15(1): 32-41, PMID: 25730650
Moore CD, Craven BC, Thabane L, Laing AC, Frank-Wilson AW, Kontulainen SA, Papaioannou A, Adachi JD, Giangregorio LM
Brain and Spinal Cord Rehabilitation Program, Toronto Rehabilitation Institute, University Health Network.
Abstract
BACKGROUND: Atrophy and fatty-infiltration of lower-extremity muscle after spinal cord injury (SCI) predisposes individuals to metabolic disease and related mortality.
OBJECTIVES: To determine the magnitude of atrophy and fatty-infiltration of lower-extremity muscles and related factors in a group of individuals with chronic SCI and diverse impairment.
METHODS: Muscle cross-sectional area and density were calculated from peripheral quantitative computed tomography scans of the 66% site of the calf of 70 participants with chronic SCI [50 male, mean age 49 (standard deviation 12) years, C2-T12, AIS A-D] and matched controls. Regression models for muscle area and density were formed using 16 potential correlates selected a priori.
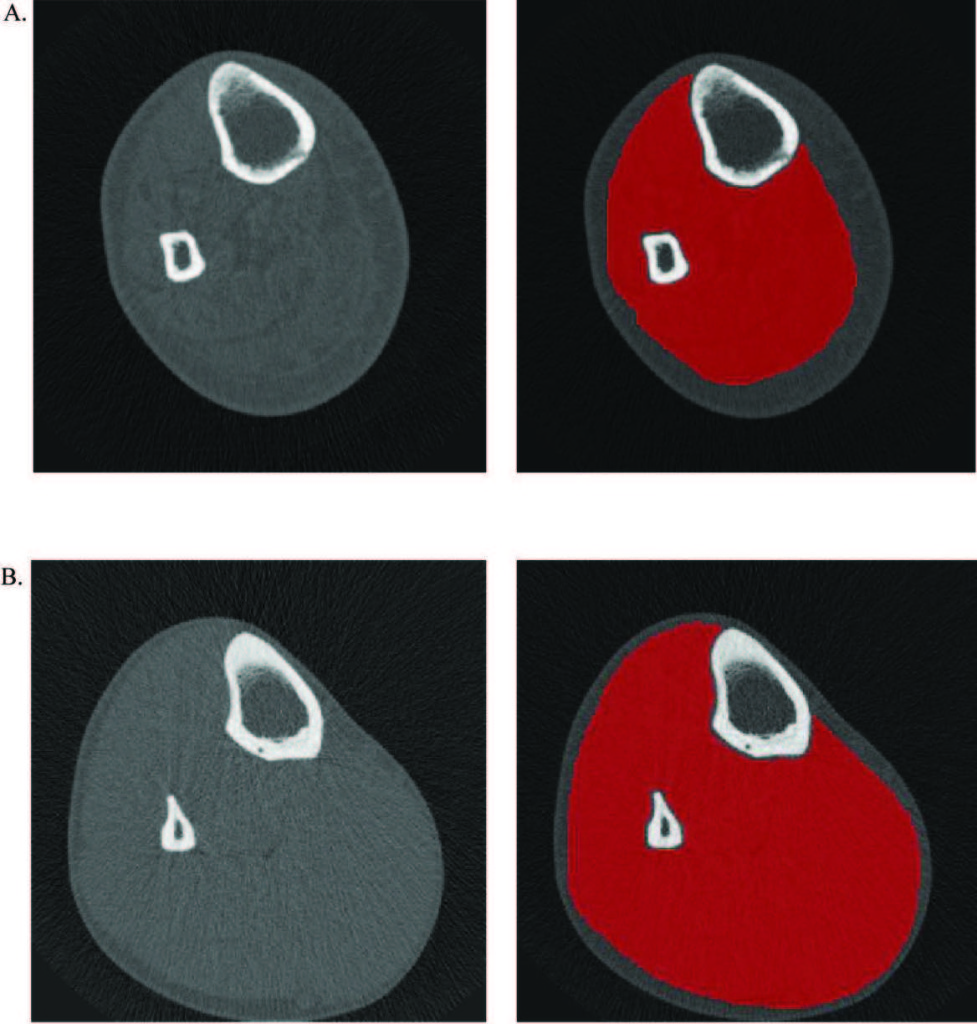
An illustration of watershed-guided muscle segmentation of the 66% site of the calf of a male with complete paraplegia (A) and corresponding able-bodied control (B).
RESULTS: Participants with motor-complete SCI had approximately 32% lower muscle area, and approximately 43% lower muscle density values relative to controls. Participants with motor-incomplete SCI had muscle area and density values that were both approximately 14% lower than controls. Body mass (+), tetraplegia (+), motor function (+), spasticity (+), vigorous physical activity (+), wheelchair use (-), age (-), and waist circumference (-) were associated with muscle size and/or density in best-fit regression models.
CONCLUSIONS: There are modifiable factors related to muscle size, body composition, and activity level that may offer therapeutic targets for preserving metabolic health after chronic SCI.